Clinical Exercise: Resuscitative Thoracotomy
Scenario:
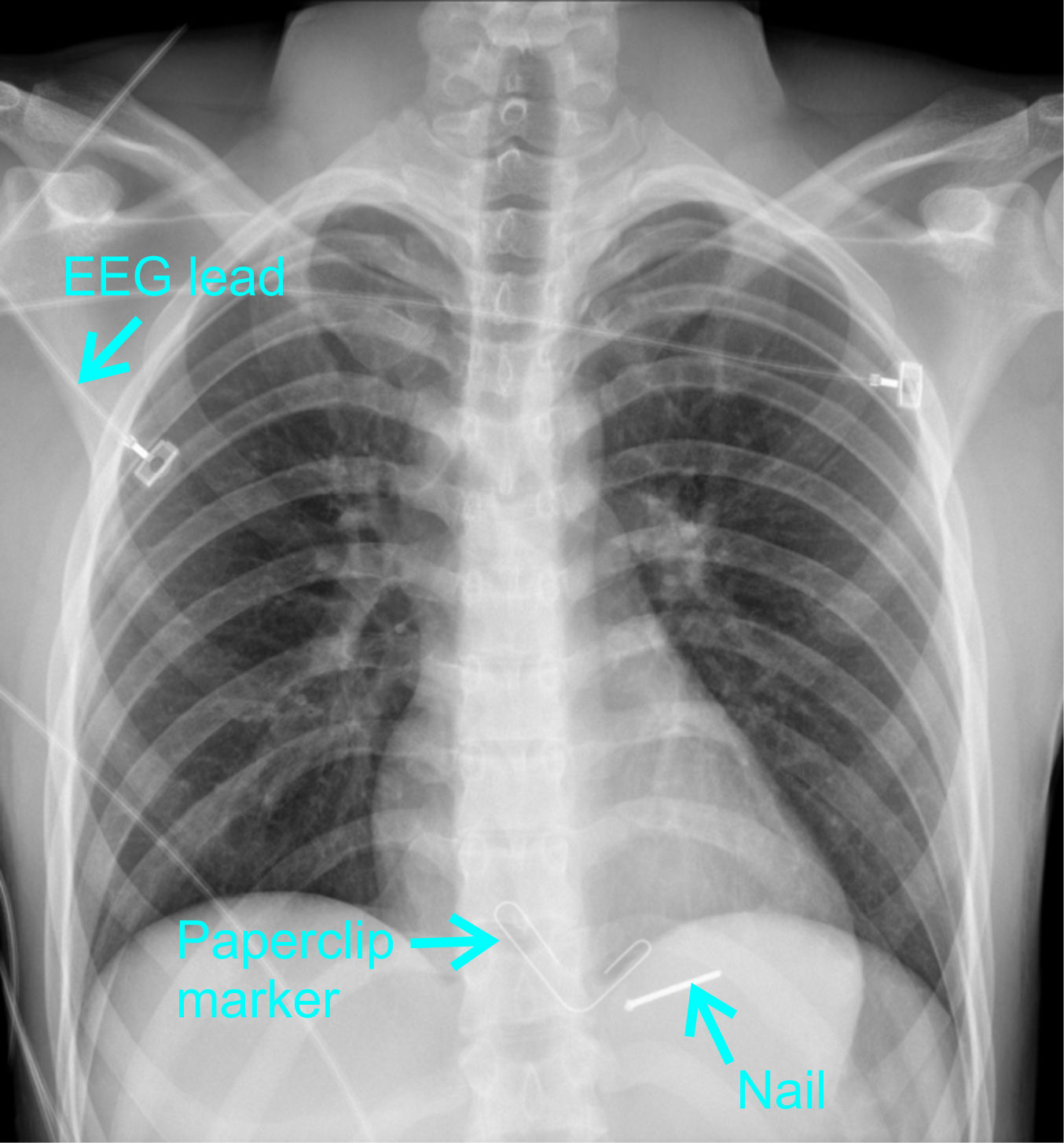
A 30 year old patient is brought into the emergency room by a co-worker after suffering an accident with a nail gun while constructing a barn. The patient is in pain but otherwise appears stable. Upon examining the patient's chest you see a small entry wound at the fifth intercostal space with no exit wound, suggesting that the nail is embedded in the patient's chest.
You perform an X-ray and observe the nail entered at an angle and the tip may have penetrated the pericardium.
As you are examining the X-ray and the charge nurse is monitoring the patient's blood pressure, the patient suddenly complains of acute chest pain and displays shortness of breath before rapid loss of consciousness. The charge nurse reports a dramatic drop in systolic blood pressure and upon listening to the patient's chest you hear only muffled heart sounds.
Diagnosis:
Any penetrating injury to the mid thoracic region are considered high-risk for serious cardiac complications. In emergency medicine, this is called 'the cardiac box' described as an arbitrary box with the upper border at the sternal notch, the lower border at the xiphoid process, and the lateral sides at the mid-clavicular line (or lateral border at the nipples). As a clinical concept, any injury within this box could lead to heart and/or great vessel injury with complications including cardiac tamponade, myocardial contusion, and hemorrhage.

The combination of a rapid drop in blood pressure and muffled heart sounds suggests the nail within the pericardium has resulted in a major cardiovascular injury. The nail itself may have been 'plugging' a hole in the heart or a coronary artery and become dislodged.
You realize the patient has developed cardiac tamponade and is entering acute cardiac arrest. You need to gain rapid access to the heart. Calling for your team you decide it is essential to perform a resuscitative thoracotomy.
Mechanism:
The condition of cardiac tamponade occurs when there is increased pressure on the heart from effusion of fluid in the pericardial space. The pericardium is an inelastic sac containing the heart that normally has only a thin film of fluid for lubrication. Excessive fluid will compress against the heart impeding the ability of the heart to pump blood.
If fluid builds up slowly the pericardium will expand and signs of the condition may be subtle and slow in onset. In this scenario the nail has induced bleeding occurring acutely into the pericardial space (bleeding into the pericardium is called hemopericardium).
The pressure of blood entering the pericardial space is compressing the heart reducing the amount of blood filling the heart and thus limiting the blood pumped with each heart beat resulting in a rapid drop in blood pressure. You will also observe swelling (distention) of the jugular veins due to an increase in pressure in the pericardium preventing venous blood from returning into the heart. The heart sounds are being muffled by the fluid buildup inside the pericardium.
This combination of signs, called Beck's Triad, of a drop in blood pressure, jugular distension, and muffled heart sounds are the classic signs of cardiac tamponade.
Treatment (perform these steps on the donor in a mock-procedure):
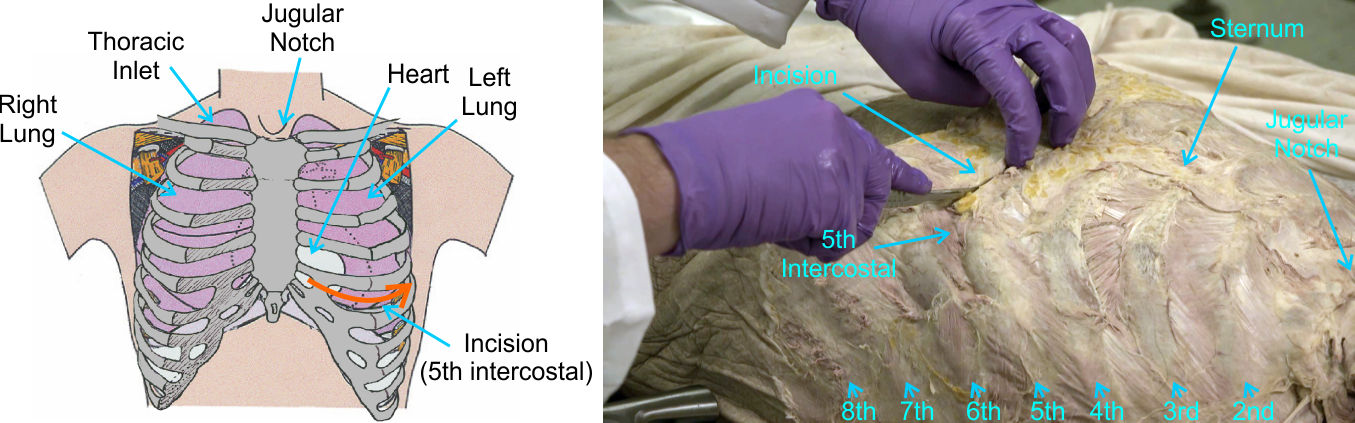
To treat this patient you need to gain access to the heart to relieve the pericardial pressure and equally importantly gain access to the site of aortic bleeding. The fastest way to gain such access is through a resuscitative thoracotomy, which is also known as an Emergency Department Thoracotomy (EDT). More formally the approach is a unilateral anterolateral thoracotomy (itself known in surgical slang as a 'hemi-clamshell' thoracotomy).
The goal of this procedure is to enter the space between two ribs and spread the ribs apart sufficiently to get instruments or your hand into the thoracic cavity to access the heart.
This approach clearly compromises pulmonary function since chest-expansion respiratory mechanisms can no longer occur. Thus, before any thoracotomy is performed on a living patient the airway is controlled with endotracheal intubation such that the patient's lungs can be artificially expanded/contracted by force ventilation. In addition, wide bore intravenous access is obtained to delivery large volumes of replacement fluid to compensate for the severe blood volume loss from the bleeding.
PREPARATION: You will need the Finochietto rib spreader and Lebsche knife from the tool tray under your table.
1) Position the patients left arm out to the side such that you have adequate access to the anterolateral thoracic wall.
2) In a patient you would make an incision inferior to the breast through the skin, subcutaneous tissue, and any portions of the pectoralis major muscle.
As you have already removed superficial tissues proceed to the next step.
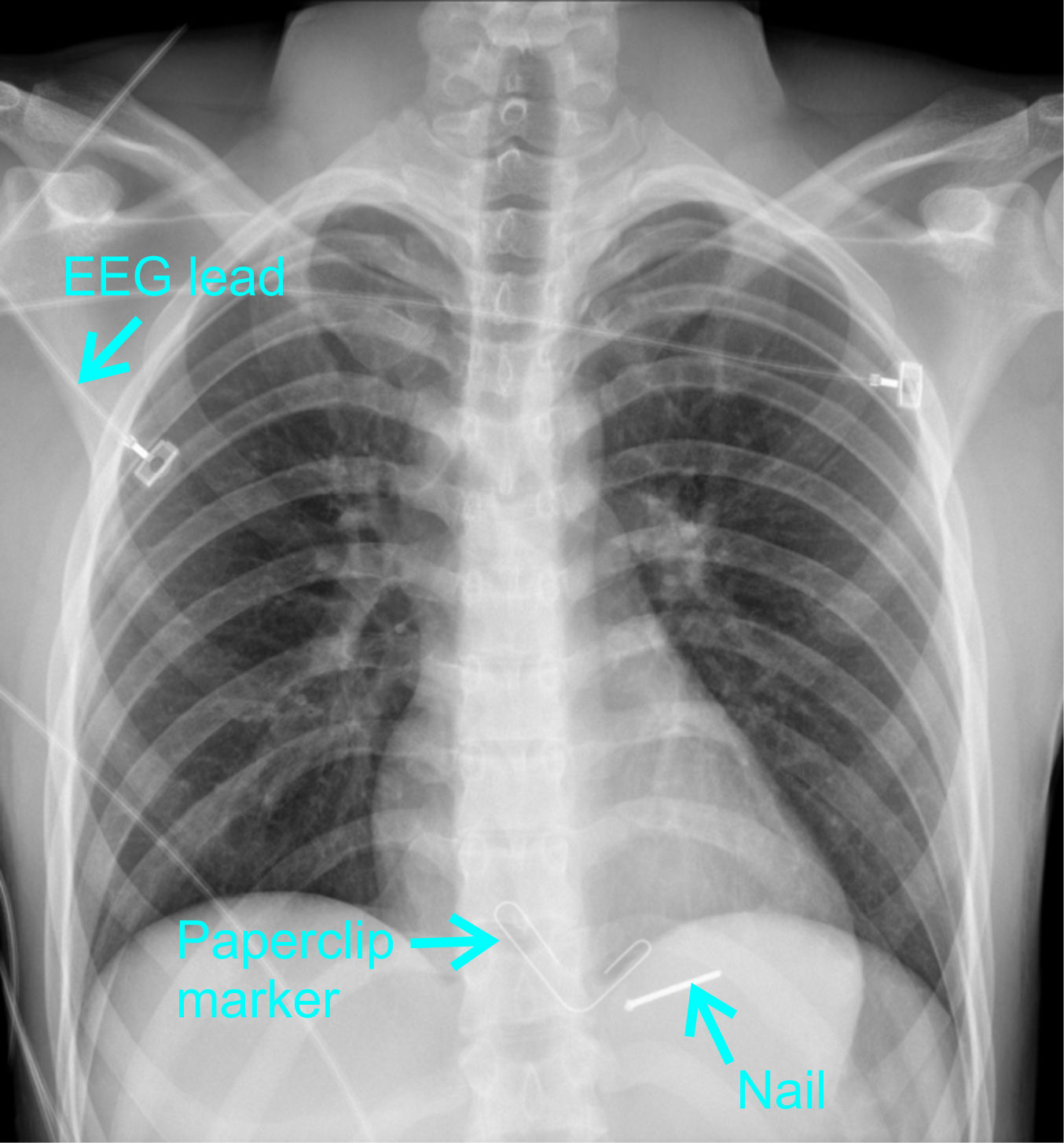
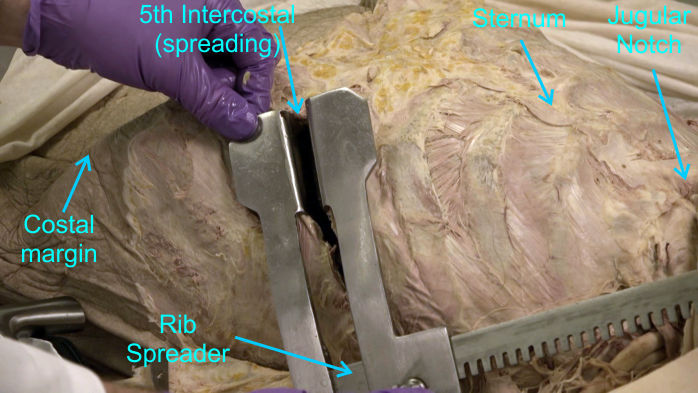
3) With your fingers identify the 5th intercostal space (the soft tissue gap between ribs 5 and 6).
Since this is an emergency procedure with time of the essence in the living, surgeons will accept a 'best guess' intercostal space since either the 4th or 5th space will give suitable access.
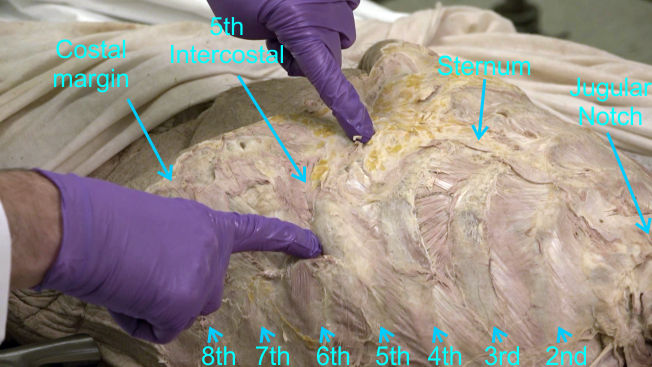
4) Near to the sternum use a scalpel to make a small incision all the way through the intercostal muscles.
5) Place one blade of scissors through the incision and extend the incision laterally to the left following the 5th intercostal space as far as the mid-axillary line.
In the living, you would usually insert a finger into the gap while cutting in order to push the lung away minimizing risk of lung penetration by the scissors.
6) Insert the blades of the rib spreader between the ribs.
Commonly, the handle of the spreaders is oriented to the lateral side. This facilitates conversion from a unilateral (hemi-clamshell) thoracotomy to a bilateral (full clamshell) thoracotomy if necessary.
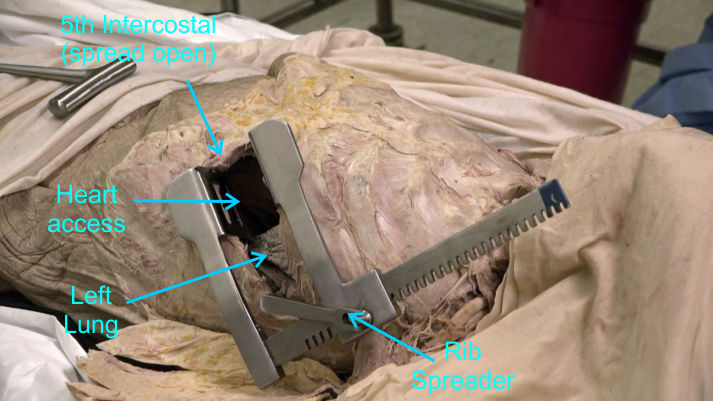
7) Using the ratchet handle spread the gap between the ribs in order to expose the thoracic organs.
Look into the opening and observe the inferior aspect of the lung on the left and the surface of the pericardium towards the midline. The amount of access to the heart through an anterolateral thoracotomy can be limited depending on the patient's thoracic stature and size of their heart.
Scenario (addendum):
After opening the anterolateral aspect of the thoracic cavity you realize that the degree of access will be insufficient to rapidly and efficiently control the aortic hemorrhaging. In considering your options at this time you decide the best choice of action to improve access is to continue the incision across to the right anterolateral thorax to convert the opening into a bilateral anterolateral thoracotomy (a full-clamshell opening).
Treatment (continued):
8) Place the Lebsche knife at the medial end of your thoracotomy opening cut transversely through the sternum and the corresponding intercostal space.
Use one hand on the grip handle of the Lebsche knife to keep the blade 'aimed' at the corresponding intercostal space on the other side of the sternum while advancing the blade with hammer impacts.
Ensure everyone has the opportunity to use the Lebsche knife. Swap roles halfway through the sternum so a second person can use the Lebsche knife to go through the remainder of the sternum.
There will be a second use of the Lebsche to cut through the manubrium later in the lab, so the remaining team members will get to use the Lebsche for that superior sternal cut.
There are two significant vessels running immediately deep to the sternum, the internal thoracic arteries, that are transected with this approach. In the living, due to profound hypotension necessitating the resuscitative thoracotomy there is typically minimal bleeding during the procedure. However, these vessels would need to be clamped later to minimize bleeding once cardiac output and blood flow is restored. We will examine those vessels later in the lab session.
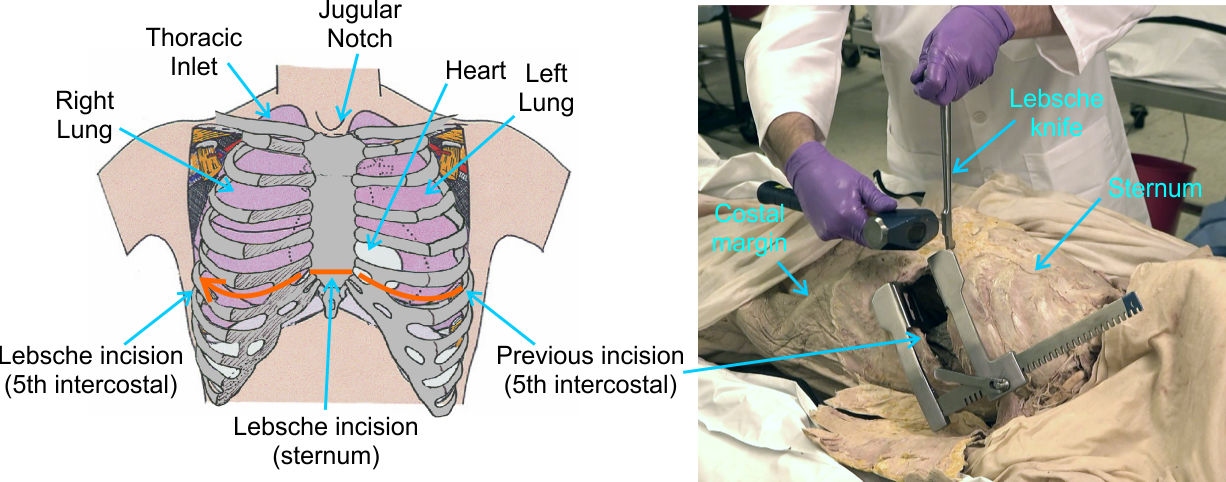
9) Place one blade of scissors (or a scalpel) and extend the incision laterally on the right following the 5th intercostal space as far as the mid-axillary line.
10) Reposition the rib spreaders and using the ratchet handle spread the gap between the ribs elevating the sternum.
There are often adhesions of fatty tissue or membranes to the chest plate. If you spot such adhesions, use your fingers to force/tear them as close to the chest plate as you can to leave most of the membranes with the thoracic contents.
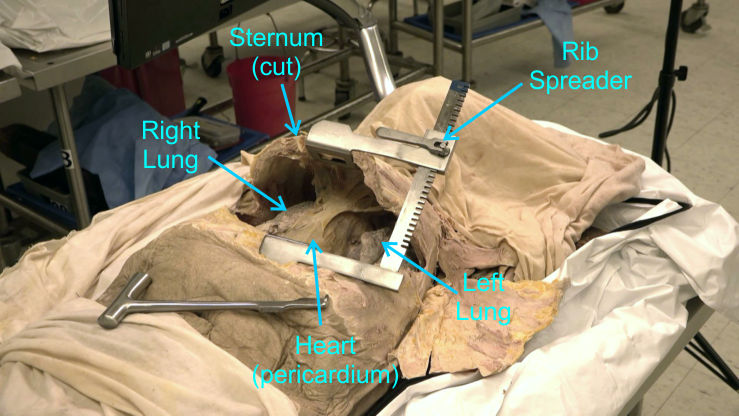
11) Observe into the opening and observe the left and right lungs and the surface of the pericardium at the midline.
Ensure everyone has had the opportunity to use the rib spreaders (remove the spreader and replace as needed) before completing the exercise and returning to the lab procedures.
Outcome:
The bilateral resuscitative thoracotomy provides sufficient access for controlling the aortic bleeding and releasing the cardiac tamponade (surgical procedures for a later training session). Cardiac output and blood pressure return to normal ranges. After closing the chest the patient requires considerable convalescence, but she recovers fully and is able to return to work building barns.