Clinical Exercise: Tube Thoracostomy
Scenario:
A 28 year old patient is brought into the emergency room after a motor vehicle crash. He describes to the emergency team that he is short of breath and the right side of his chest hurts.
Examination reveals a rapid heart rate, low blood oxygen levels, low blood pressure, rapid respiration, and markedly diminished breathing sounds from the right side of the chest. Evaluation of the patient's airways and the patient's ability to vocalize indicate the upper airways are clear.
Diagnosis:
You recognize that the patient is in acute respiratory distress. A percussive tap to the patient's chest reveals a hollow drum-like sound from the right compared to the normal duller tone from the left side. Coupled with the diminished breathing sounds from the right indicate the patient is suffering a tension pneumothorax and an immediate insertion of a chest tube (tube thoracotomy) is required to evacuate excess air and fluids from the plural space.
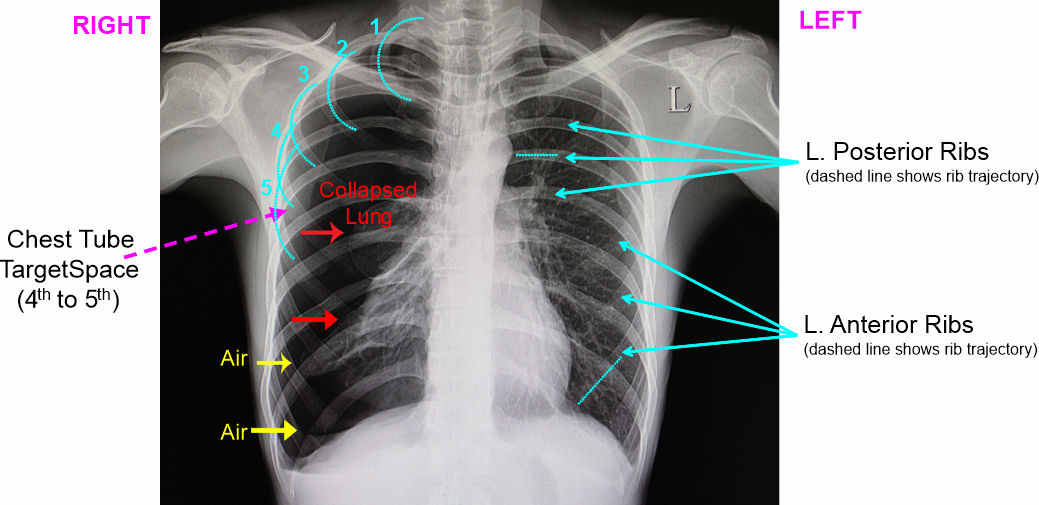
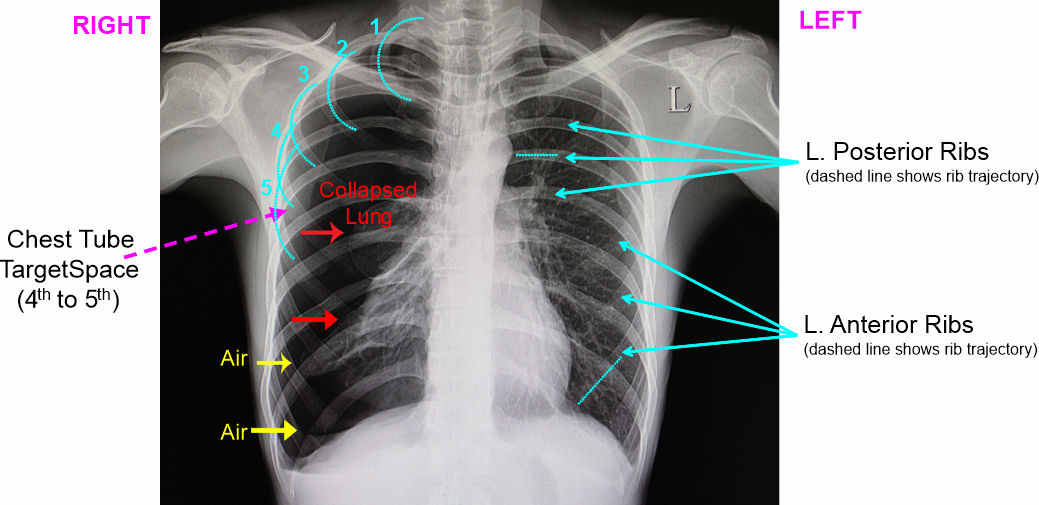
A chest X-ray (CTX) can confirm the diagnosis (although in acute cases there may be insufficient time to get a chest X-ray before intervention must occur).
On a CTX, the normal lung has a lacy white strand-like appearance within the pleural cavity (in the image below left lung). The strand like appearance is the slightly higher density of vessels/airways within the lung creating a lace-like pattern. On the affected side, lung tissue is collapsed towards the mediastinum (on the image below the right lung) with the lacy area collapsed close into the mediastinum. Additionally, the space previously occupied by the lung is now air filled, so the affected side lateral pleural cavity is a hypodense (darker) air filled space. Thus, the terminology of a 'pneumo..' (air), '..thorax' (chest).
Mechanism:
A tension pneumothorax is a result of a violation of the visceral pleura resulting in a pulmonary injury and air leak into the pleural space. The air accumulates in the affected space compressing the lung and shifting the mediastinum towards the contralateral side. This shift results in compression of the lung on the other side and compression posteriorly on the vena cava. Untreated, this will result in acute hypoxia (lack of oxygen) and hypotension (low blood pressure) from the impaired venous return.
A thoracostomy is a small incision in the chest wall in which the opening is maintained for drainage, usually by insertion of a thoracostomy needle or thoracostomy tube (chest tube).
Treatment (perform these steps on the donor in a mock-procedure):
PREPARATION: Send a member of your team to the instrument supply tables to fetch two of the plastic thoracotomy tubes so that members of the team can work on both the left and right side at the same time (please take only the supply numbers indicated to ensure sufficient supplies are available for all tables).
Prepare two scalpels (typically two are all that are needed, the extra scalpel handles in your draw are useful tools for positioning when not equipped with a blade)
1) With the patient in the anatomic position, estimate the location on the lateral thoracic wall that is opposed to the halfway point along the humerus from the acromion (tip of shoulder) to the elbow...this anatomic relationship identifies the 4th to 5th rib location in almost all patients regardless of stature.
Use a marker pen to demarcate this position on the chest wall such that when you move the arm out of the way you will not lose track of the incision location. In the living, the area would be cleaned with a disinfectant and a local anesthesia injected.
The level of the nipple is often used as a guide to position, however nipple position is variable between individuals and subject to considerable inaccuracy in the obese patient. The humerus-to-ribcage relationship is more consistent.
The vicinity of the 4th/5th ribs at the lateral thorax is a "safe zone" for access, as the zone is located posterolateral to the pectoralis major muscle, anterior to the latissimus dorsi muscle, and inferior to important nerves/arteries in the axilla (armpit).

2) Make a small incision through the skin approximately 4-5cm long parallel to the ribs.
If your patient has abundant subcutaneous tissue a longer incision to the 6-10cm length will make access easier.
3) Using hemostats (locking forceps) in a spreading motion, part the skin and subcutaneous tissue to widen the opening.
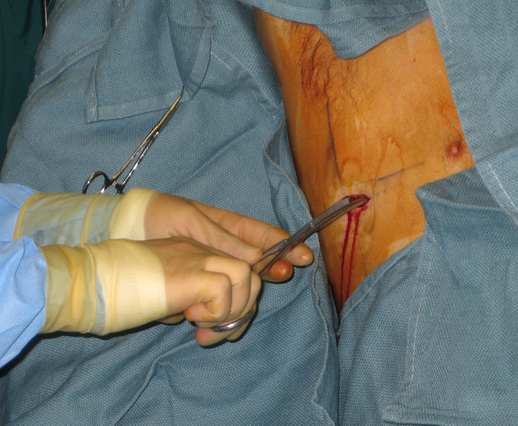
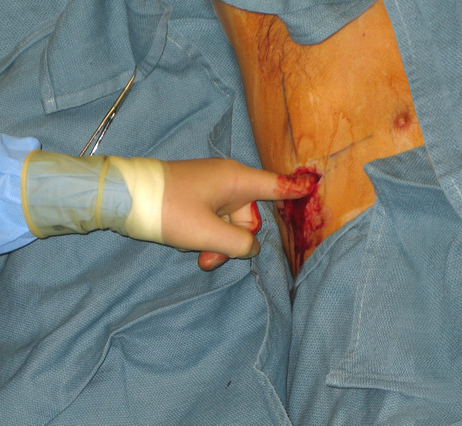
4) Force your finger into the opening and spread subcutaneous tissue sufficiently to feel the ribs.
5) Using hemostats, push the closed end through the intercostal muscles and spread the hemostats forcefully open to form a hole in the intercostal muscles.
This maneuver requires some force and twisting motion of the hemostats to gain entry through the intercostal muscles.
The intercostal muscle layer can be overly tough on the donor. If this is the case, use a scalpel to make a small opening instead.
6) Push your finger back into the space, and twisting your finger press any lung tissue back from the hole.
7) Grasp the chest tube end with forceps and feed it into the opening.
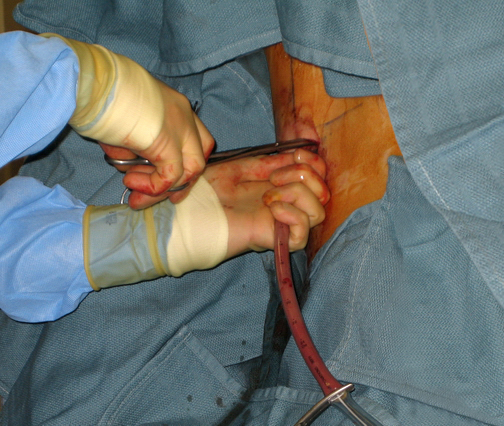
8) By releasing and then re-clamping the tube, advance the end posteriorly into the pleural space.
When inserted correctly it is common for fluid (in our case embalming fluid) to rush out of the tube.
9) After insertion, the tube is typically secured by a suture and the entry area covered by dressings (we will skip this stage).

10) Once in place, a chest X-ray is performed to verify the location of the drain. The tube will remain in place until the air is drained and risk of returning air diminishes.
Repeat the procedure on the other side of the donor so that more of your team can practice the procedure. When finished, leave the chest tubes in place on each side so that you can verify your placement precision after we open the ribcage in a later lab session.
Outcome:
The drainage of the chest decompresses the tension pneumothorax resulting in improved ventilation, oxygenation, and blood return to the heart. The patient reports they are able to breathe easier. Respiration and blood pressure rates return to more normal levels.
Images from eMedicine